Dealing with recurring yeast infections can feel frustrating and exhausting, especially when they disrupt daily life and comfort. Many women find themselves caught in a cycle of discomfort, itching, and irritation that seems to return no matter what they try. It’s a common issue that affects millions, often leading to questions about why it persists and how to manage it better. But here’s the intriguing part: there might be some unexpected everyday factors at play, and understanding them could make a real difference—stick around to uncover a lesser-known tip at the end that could change your approach.

Understanding Yeast Infections: The Basics
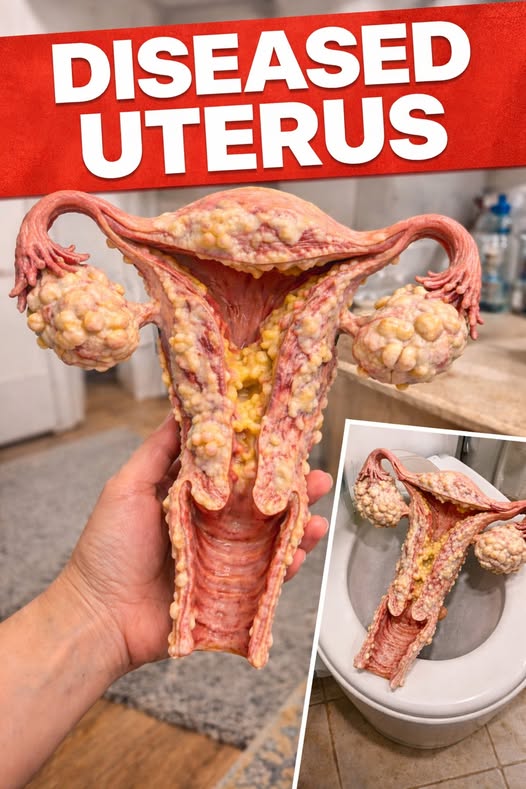
Yeast infections, also known as candidiasis, occur when there’s an overgrowth of Candida, a type of fungus naturally present in the body. This imbalance can happen in the vaginal area, leading to symptoms like itching, burning, and unusual discharge. Research from the Centers for Disease Control and Prevention (CDC) indicates that about 75% of women will experience at least one in their lifetime, with many facing recurrences.
But that’s not all. Recurring infections might signal underlying habits or conditions that encourage yeast growth. Let’s dive into the surprising reasons behind this persistence.
Reason 1: Antibiotic Use and Its Hidden Impact
Antibiotics are lifesavers for bacterial infections, but they can disrupt the body’s natural balance. By killing off good bacteria along with the bad, they create an environment where yeast can thrive unchecked. Studies published in the Journal of Antimicrobial Chemotherapy show that women taking broad-spectrum antibiotics have a higher risk of developing yeast infections shortly after.
Here’s where it gets interesting. Even short courses of antibiotics for unrelated issues, like a urinary tract infection, can tip the scales. To help maintain balance, consider discussing probiotic options with your healthcare provider during antibiotic treatment.
- Incorporate yogurt with live cultures into your diet.
- Stay hydrated to support overall microbial health.
- Monitor symptoms closely after finishing antibiotics.
Reason 2: Hormonal Fluctuations Throughout Life Stages
Hormones play a big role in the body’s ecosystem, and shifts can promote yeast overgrowth. During pregnancy, estrogen levels rise, increasing glycogen in the vagina, which yeast loves to feed on. Similarly, birth control pills or hormone replacement therapy can mimic these changes.
The truth is, even menstrual cycles cause minor fluctuations that some women notice as recurring issues around their period. A review in the American Journal of Obstetrics and Gynecology highlights how these hormonal ebbs and flows contribute to vulnerability.
Simple steps like tracking your cycle with an app can help you anticipate and prepare. Opt for breathable cotton underwear during high-risk times to reduce moisture buildup.

Reason 3: Uncontrolled Blood Sugar Levels
High blood sugar provides a feast for yeast, as Candida thrives on glucose. Women with diabetes or prediabetes are particularly susceptible, but even occasional spikes from a sugary diet can contribute. According to the National Institute of Diabetes and Digestive and Kidney Diseases, elevated glucose levels in bodily fluids encourage fungal growth.
But wait, there’s more. Stress-induced cortisol can also raise blood sugar indirectly. Managing this involves monitoring your intake of refined carbs and sweets.
Try these actionable tips:
- Choose whole grains over processed foods.
- Include protein in every meal to stabilize blood sugar.
- Regular exercise, like a daily walk, can help regulate levels.
Reason 4: Clothing Choices That Trap Moisture
Tight-fitting clothes, especially synthetic fabrics like nylon, can create a warm, moist environment ideal for yeast. Jeans, leggings, or non-breathable underwear worn for long periods trap heat and sweat, disrupting the natural pH balance.
Research from the British Journal of Dermatology suggests that moisture-retaining clothing increases the likelihood of infections in humid climates or during workouts. This is especially relevant for active women or those in warm environments.
Switching things up is straightforward. Go for loose, cotton-based attire, particularly in the lower body. After exercising, change out of sweaty clothes promptly to keep things dry.
Reason 5: Hygiene Products and Their Unintended Effects
Scented soaps, douches, and feminine sprays might seem helpful, but they can irritate sensitive areas and kill off beneficial bacteria. These products alter the vaginal pH, making it more hospitable to yeast. The American College of Obstetricians and Gynecologists advises against douching, noting it can lead to imbalances.
And here’s a key point: even bubble baths or scented toilet paper can be culprits. Opting for gentle, unscented alternatives is a smart move.
Follow this step-by-step guide:
- Choose fragrance-free, pH-balanced cleansers for external use only.
- Pat dry gently after bathing instead of rubbing.
- Avoid introducing any products inside the vagina.

Reason 6: Dietary Habits Fueling the Cycle
A diet high in sugar and refined carbohydrates feeds yeast directly, as these break down into simple sugars. Processed foods, sodas, and even some fruits in excess can contribute to overgrowth. Studies in the journal Nutrients link high-glycemic diets to increased Candida presence.
But that’s not the end of it. Alcohol and caffeine might indirectly affect gut health, which influences vaginal flora. Balancing your plate with veggies, proteins, and healthy fats can make a difference.
| Food Type | Examples | Why It Helps or Hurts |
|---|---|---|
| To Limit | Candy, white bread, soda | Provides quick sugar for yeast |
| To Include | Leafy greens, nuts, lean proteins | Supports balanced microbiome |
| Neutral Options | Whole fruits in moderation | Natural sugars but with fiber |
Reason 7: Weakened Immune System Factors
A compromised immune system from stress, lack of sleep, or illnesses like HIV can allow yeast to flourish. Chronic stress raises cortisol, which suppresses immune responses. The World Health Organization notes that lifestyle factors significantly impact immune health and infection susceptibility.
The fascinating aspect? Even seasonal allergies or autoimmune conditions can play a role by diverting immune resources.
Boost your defenses with these habits:
- Aim for 7-9 hours of sleep nightly.
- Practice stress-relief techniques like meditation.
- Eat immune-supporting foods rich in vitamins C and D.
Reason 8: Sexual Activity and Partner Transmission
While not a sexually transmitted infection, yeast can pass between partners during intimacy, especially if one has an active overgrowth. Uncircumcised partners or those with poor hygiene might harbor yeast. A study in the New England Journal of Medicine discusses how recurrent infections can sometimes involve reinfection from partners.
Yet, communication is key. Using barriers like condoms can reduce transmission risks.
Discuss openly with your partner about hygiene practices. Both maintaining good personal care routines can help prevent back-and-forth issues.
Practical Strategies to Support Vaginal Health
Beyond identifying reasons, incorporating daily habits can promote a healthier balance. Probiotics, found in foods like kefir or supplements, may support beneficial bacteria, as suggested by research in the Journal of Clinical Gastroenterology.
Stay consistent with these tips:
- Drink plenty of water to flush the system.
- Wipe from front to back after using the bathroom.
- Avoid hot tubs or very hot baths that can encourage warmth-loving yeast.
And remember that lesser-known tip I mentioned earlier? Incorporating fermented foods like sauerkraut into your diet can introduce natural probiotics without supplements, potentially aiding in maintaining flora balance—give it a try and see how your body responds.
Wrapping It Up: Empowering Your Wellness Journey
Recurring yeast infections stem from a mix of lifestyle, hormonal, and environmental factors, but awareness is the first step toward better management. By recognizing these triggers and adopting supportive habits, many women find ways to reduce their frequency. Always consult a healthcare professional for personalized advice.
Frequently Asked Questions
What lifestyle changes can help with recurring yeast infections? Focusing on breathable clothing, a balanced diet low in sugars, and good hygiene practices can support overall vaginal health. Tracking patterns and discussing with a doctor ensures tailored insights.
Are there natural ways to support balance during hormonal changes? Yes, maintaining hydration, incorporating probiotics through food, and managing stress can be helpful during periods, pregnancy, or menopause. Research supports these as general wellness strategies.
When should I see a doctor about yeast infections? If symptoms persist despite over-the-counter options or recur frequently, a healthcare visit can rule out other conditions. It’s important for accurate assessment and guidance.
Disclaimer: This article is for informational purposes only and not a substitute for professional medical advice. Consult your healthcare provider for any health concerns.