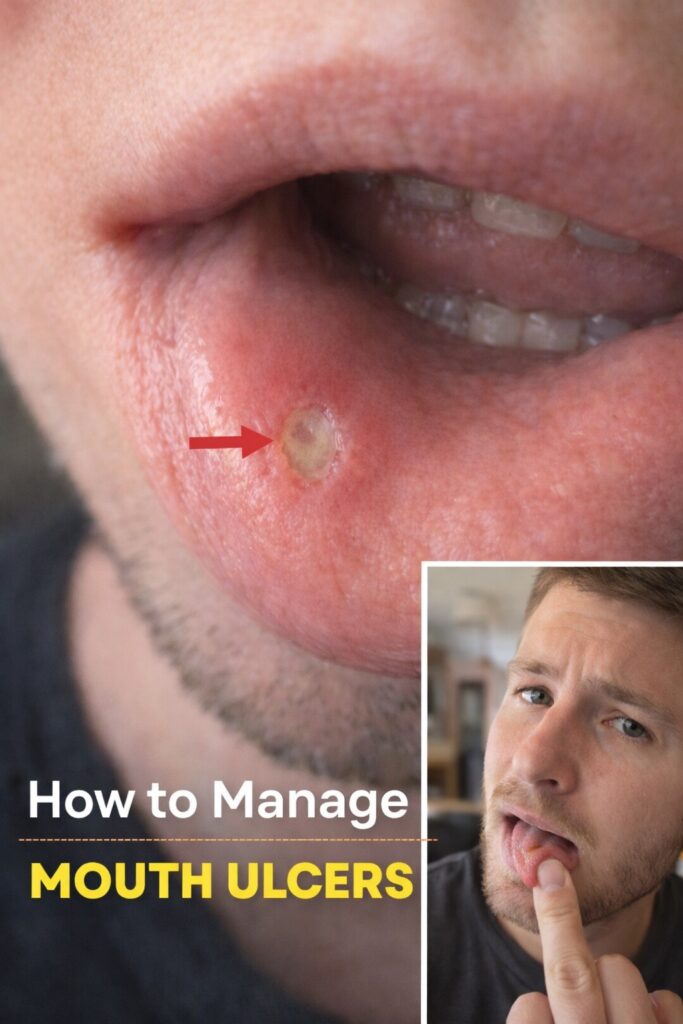
Aphthous stomatitis — commonly known as canker sores — is the most frequent type of painful ulcer that appears inside the mouth. These small, shallow, round or oval sores develop on soft tissues such as the inner cheeks, lips, tongue, gums, floor of the mouth, or soft palate. They are not contagious and are not caused by the herpes virus (unlike cold sores).
Most people experience their first canker sore between ages 10–40, but they can occur at any age. For some, they appear only once or twice in a lifetime; for others, they become recurrent (3–6+ times per year) and significantly affect quality of life.
Key Characteristics of Canker Sores
| Feature | Typical Description |
|---|---|
| Appearance | Round/oval, white or yellowish center, bright red inflamed border |
| Size | Minor: 3–10 mm (most common) Major: >10 mm (deeper, longer healing) Herpetiform: multiple tiny ulcers (1–3 mm) |
| Pain level | Moderate to severe — especially when eating, drinking, talking, or brushing teeth |
| Location | Inside mouth only (never on lips, gums outside, or skin) |
| Duration | Minor: 7–14 days Major: 2–6 weeks Herpetiform: 7–14 days |
| Healing | Heals without scarring (except major ulcers) |
| Recurrence | 20–40% of people experience recurrent episodes |
8 Most Common Triggers & Risk Factors
- Minor physical trauma
Biting the cheek, sharp tooth, dental work, aggressive brushing, braces, or ill-fitting dentures. - Stress & emotional upset
Very strong link — many people get outbreaks during high-stress periods (exams, grief, work pressure). - Nutritional deficiencies
Low levels of iron, vitamin B12, folate, zinc, or vitamin D are found in 10–30% of recurrent cases. - Certain foods & additives
Acidic/spicy foods (citrus, tomatoes, pineapple), chocolate, coffee, nuts, gluten (in celiac disease), sodium lauryl sulfate (SLS) in toothpaste. - Hormonal fluctuations
Many women notice outbreaks right before or during menstruation. - Immune system changes
Colds, flu, or starting/stopping immunosuppressive drugs can trigger episodes. - Underlying health conditions
Celiac disease, Crohn’s disease, Behçet’s disease, reactive arthritis, HIV, cyclic neutropenia. - Genetic predisposition
Strong family history is common — if parents had recurrent canker sores, risk is significantly higher.
When to See a Doctor or Dentist
Routine check (within 1–2 weeks) if:
- Sores last >2 weeks
- New sores appear before old ones heal
- Extremely painful or large (>1 cm) ulcers
- Frequent outbreaks (>6–8 per year)
- Sores accompanied by fever, swollen lymph nodes, or skin/genital ulcers
Urgent evaluation if:
- Sores appear with difficulty swallowing/breathing
- Persistent white/red patches that do not heal
- Unexplained weight loss, fatigue, or night sweats
Effective Ways to Manage & Reduce Canker Sores
Immediate pain relief
- Topical numbing gels (lidocaine, benzocaine — e.g., Orajel, Anbesol)
- Salt water rinse (½ tsp salt in warm water) 3–4×/day
- Baking soda paste (small amount on sore for 1–2 min)
- Milk of magnesia dabbed on sore (coats & neutralizes acid)
Healing accelerators
- Vitamin B12 (1,000 mcg sublingual daily) — studies show significant reduction in frequency & duration
- Zinc lozenges (10–15 mg every few hours during outbreak)
- Licorice root extract (deglycyrrhizinated licorice/DGL) — soothing & healing
- Aloe vera gel (pure) — apply directly to sore
Long-term prevention strategies
- Switch to SLS-free toothpaste (most major brands now offer SLS-free versions)
- Avoid known trigger foods (acidic, spicy, rough-textured)
- Manage stress (meditation, yoga, adequate sleep)
- Correct deficiencies (B12, iron, folate, zinc — get blood tests)
- Maintain excellent oral hygiene (soft brush, gentle flossing)
- Consider probiotics (oral strains like Lactobacillus reuteri) — emerging evidence for reducing recurrence
Bottom Line
Canker sores are painful and annoying but almost always benign. The vast majority heal within 7–14 days without complications. However, frequent, severe, or prolonged ulcers are not “normal” and deserve investigation — especially after age 40–50 when other oral conditions (including precancerous changes) become more common.
Quick action checklist
- Switch to SLS-free toothpaste today
- Try salt water rinses 3–4×/day during an outbreak
- Consider sublingual vitamin B12 (1,000 mcg daily) for 2–3 months
- Track frequency & triggers in a small notebook
- If outbreaks are >6/year or last >2 weeks → see a dentist or oral medicine specialist
Disclaimer
This article is for informational purposes only and is not medical or dental advice. Persistent, severe, or recurrent oral ulcers can be a sign of serious conditions (Behçet’s disease, Crohn’s, celiac, oral cancer, autoimmune disorders, etc.). Any sore lasting >2 weeks, accompanied by unexplained weight loss, fever, swollen lymph nodes, or skin/genital ulcers requires prompt professional evaluation. Never self-diagnose or delay care based on this list. Personalized assessment by a dentist, oral medicine specialist, or physician is essential. Early diagnosis dramatically improves outcomes.