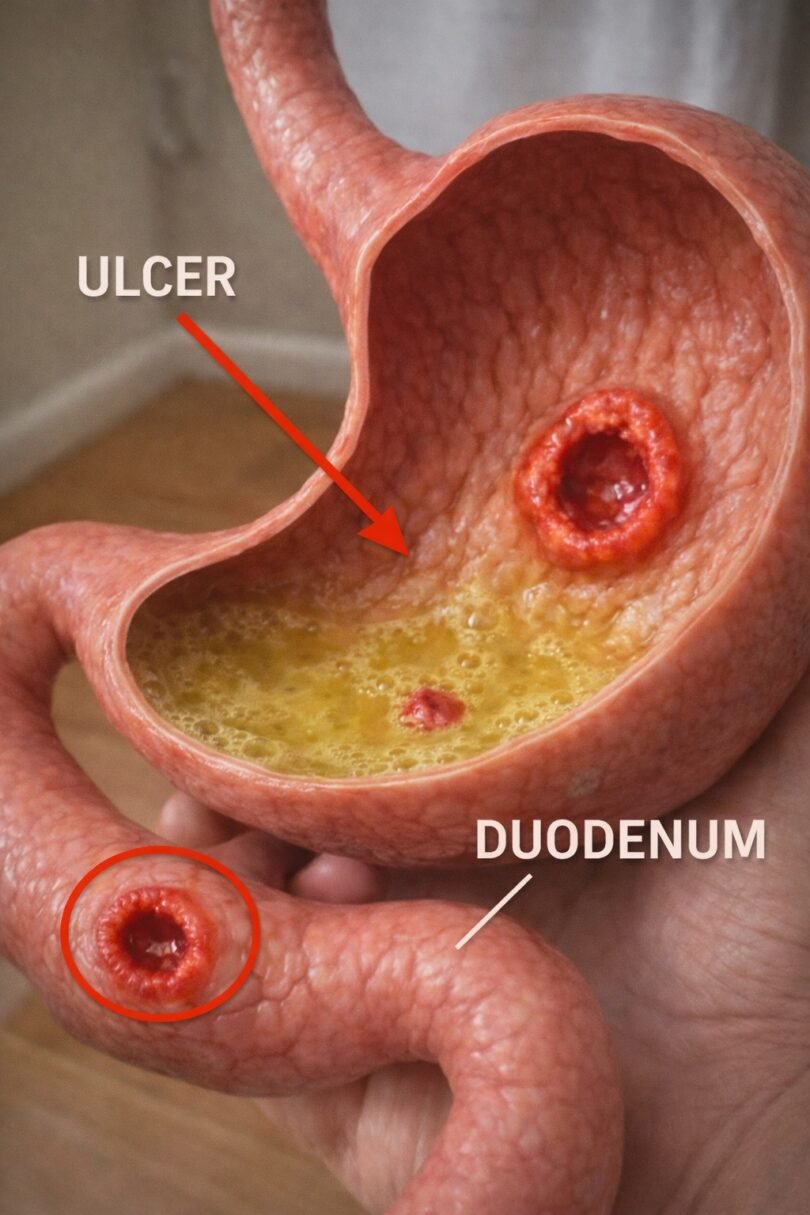
Foods to Avoid If You Want Your Peptic Ulcer to Have the Best Chance to Heal
Living with a peptic ulcer — whether in your stomach or duodenum — can feel frustrating and painful. That burning sensation, the bloating, the discomfort that interrupts your day… it’s exhausting. Many people find that even while following their doctor’s treatment plan, certain everyday foods seem to make symptoms flare up and slow down the recovery process. Research from trusted sources like the Mayo Clinic and WebMD shows that while food doesn’t cause ulcers, specific choices can irritate the lining and increase discomfort. But here’s the encouraging part: making thoughtful adjustments to what you eat might give your body the supportive environment it needs during healing — and there’s one surprising everyday habit that could be holding you back more than you think (keep reading to discover it).

Why Your Diet Matters More Than You Might Expect
Peptic ulcers are open sores in the digestive tract lining, often linked to H. pylori bacteria or long-term NSAID use. Modern understanding, backed by studies from institutions like the National Institute of Diabetes and Digestive and Kidney Diseases, emphasizes that diet plays a supportive role in symptom management. Certain foods and drinks can stimulate acid production, delay digestion, or directly irritate sensitive areas, making it harder for the tissue to recover comfortably. Everyone’s tolerance varies, so tracking your own reactions is key — but starting with common triggers is a smart first step.
The Top Foods and Drinks That May Worsen Symptoms
Here are the most frequently mentioned irritants that experts recommend limiting or avoiding when managing peptic ulcers:
- Alcohol — Even moderate amounts can erode the protective mucous layer, increase acid, and delay healing, according to Mayo Clinic guidelines.
- Caffeinated beverages (coffee, tea, energy drinks) — These stimulate acid secretion and can aggravate irritation, even decaf in some cases.
- Spicy foods (chili peppers, hot sauces, heavy seasonings) — While they don’t cause ulcers, capsaicin can cause burning and discomfort in many people.
- Fried and high-fat foods (french fries, fried chicken, fatty meats) — They take longer to digest, leading to bloating, pain, and extended exposure of the lining to acid.
- Acidic foods (citrus fruits, tomatoes, vinegar-based items) — These may trigger symptoms in sensitive individuals, especially if acid reflux is present.
- Chocolate — Contains compounds that relax the esophageal sphincter and boost acid production.
- Carbonated drinks — The fizz can cause bloating and distension, adding pressure on the stomach.
But that’s not all… The real game-changer often comes down to how these foods interact with your daily routine.
A Handy Comparison: Foods That Might Irritate vs. Gentler Alternatives
To make it easier to spot patterns, here’s a quick side-by-side look:
- Potential Irritants → Why They Might Bother You → Gentler Swap Ideas
- Alcohol → Increases acid & erodes lining → Herbal tea or water with lemon (if tolerated)
- Coffee/Strong tea → Boosts acid production → Decaf herbal options or mild green tea
- Spicy dishes → Direct chemical irritation → Mild herbs like basil or oregano
- Fried foods → Slow digestion & bloating → Baked, steamed, or grilled lean proteins
- Citrus/tomatoes → Acidic load → Bananas, melons, or apples (peeled if needed)
- Chocolate → Relaxes sphincter → Small amounts of carob if craving sweets
Pay attention to your body’s signals — what bothers one person might be fine for another.

Practical Tips to Support Your Comfort Right Now
Here are actionable steps you can try today:
- Eat smaller, more frequent meals instead of large ones to avoid overloading your stomach.
- Stop eating 2-3 hours before lying down to reduce nighttime discomfort.
- Keep a simple food journal for a week — note what you eat and how you feel afterward.
- Choose cooking methods like steaming, baking, or boiling over frying.
- Stay hydrated with plain water, but sip slowly rather than gulping.
These small shifts can make a noticeable difference in how your stomach feels day to day.

Common Questions People Ask About Ulcer-Friendly Eating
What if a food doesn’t bother me — can I still eat it? Yes, individual tolerance matters most. If something doesn’t cause pain or flare-ups for you, there’s no need to eliminate it completely.
Do I need to follow a strict “bland diet” forever? No — experts like those from Healthline note that there’s no one-size-fits-all ulcer diet. Focus on avoiding personal triggers while enjoying a balanced, nutrient-rich eating pattern.
Can certain foods actually help support healing? While no food cures ulcers, incorporating fiber-rich options like oatmeal, lean proteins, and probiotic foods (like yogurt) may promote gut balance — always discuss with your doctor.
Living with a peptic ulcer is challenging, but you’re not alone in figuring out what works best for your body. By being mindful of these common irritants and making gentle adjustments, you give your digestive system the best possible support alongside proper medical care.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider before making changes to your diet or treatment plan, especially if you have a diagnosed condition like a peptic ulcer.