9 Important Signs of Cervical Cancer Women Should Know About (And Why Regular Screening Matters)
Many women go through life noticing small changes in their body but brush them off as normal parts of aging, stress, or hormonal shifts. These subtle shifts can sometimes point to something more serious, like cervical cancer — a disease that develops slowly and often stays silent in its earliest stages. According to reliable health organizations, thousands of cases are found each year, but early attention makes a big difference in outcomes.
The good news is that cervical cancer is one of the most preventable cancers when caught through routine care. In this guide, we’ll explore key signs that experts from the Mayo Clinic and American Cancer Society often highlight, explain why they happen, and share simple steps you can take right now. Stick around until the end — there’s an important everyday habit that can help protect your health long-term.

Why Cervical Cancer Can Be Hard to Notice Early
Cervical cancer starts in the cells of the cervix, the lower part of the uterus that connects to the vagina. Most cases are linked to long-term infection with certain types of human papillomavirus (HPV), a very common virus.
Research shows that in early stages, there are often no obvious signs at all. That’s why health experts stress regular screening — it can detect changes before symptoms even appear. When the condition advances, the body may start sending clearer messages.
But here’s the key: many of these messages are easy to mistake for everyday issues like menstrual changes or minor infections. Recognizing them early and talking to a doctor can lead to quicker evaluation.

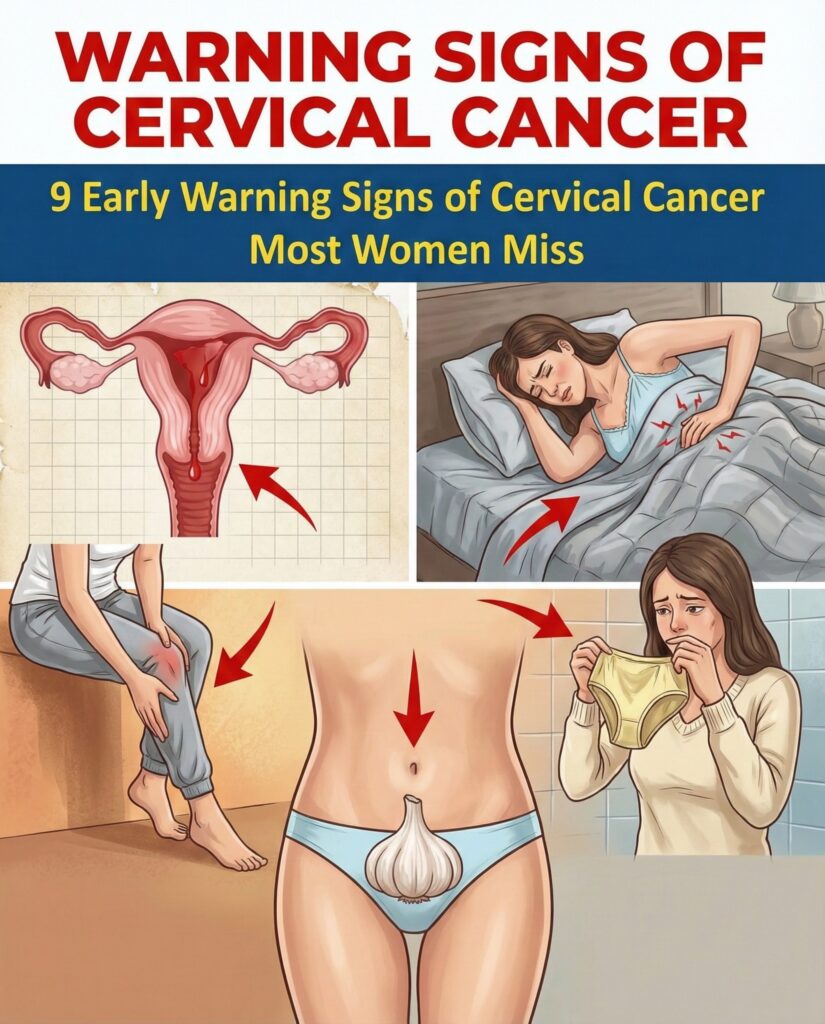
Key Signs to Pay Attention To
Health authorities like the Mayo Clinic and American Cancer Society list several changes that may appear as cervical cancer develops. Remember, these can also come from many non-cancer causes — but they deserve attention if they persist.
- Unusual vaginal bleeding — This is one of the most reported early clues. It includes spotting between regular periods, bleeding after sexual intercourse, heavier or longer periods than usual, or any bleeding after menopause.
- Changes in vaginal discharge — Normal discharge varies, but watch for watery, heavy, pink, brown, or blood-tinged discharge that has a strong or foul odor and doesn’t go away.
- Pain in the pelvic area or lower back — A persistent, dull ache that feels different from typical cramps or muscle strain and doesn’t ease with rest.
- Discomfort during or after intimacy — New or ongoing pain that may feel deep or sharp, sometimes with bleeding afterward.
These signs often appear because abnormal cells make cervical tissue more fragile, leading to easy bleeding or extra fluid production.
But that’s not all… As the condition progresses further, other changes might show up, including:
- Unexplained fatigue that feels overwhelming and doesn’t improve with sleep
- Problems with urination or bowel habits, such as more frequent urges, pain, or blood
- Swelling or pain in the legs
Again — these can have many causes. The important part is not to ignore ongoing changes.

Real Talk: Why Women Often Wait to Seek Help
Many women share similar stories: “I thought it was just hormones” or “It started so gradually I didn’t notice.” Life gets busy — work, family, stress — and small signals get pushed aside.
The truth is delaying care can allow changes to advance. On the flip side, studies highlight that when found early, the 5-year relative survival rate is around 91% (National Cancer Institute data). That’s powerful motivation to stay proactive.
Practical Steps You Can Take Today
Here are actionable ways to support your health — no big promises, just smart habits experts recommend:
- Schedule regular screenings — Follow guidelines: Pap tests every 3 years (ages 21–29) or Pap + HPV co-testing every 5 years (ages 30–65). Talk to your doctor about what’s right for you.
- Consider HPV vaccination — It’s most effective when given earlier, but ask your provider if it’s an option for you.
- Practice safe habits — Use protection during intimacy and avoid smoking, which increases risk.
- Track your body — Keep a simple note of any changes in bleeding, discharge, or pain. This helps when discussing with a doctor.
Quick self-check list:
- Have you had a screening in the last 3–5 years?
- Noticed any unusual bleeding or discharge lately?
- Feeling persistent pelvic discomfort?
If any answer raises concern, reach out to a healthcare professional soon.
What Happens Next? A Simple Action Plan
Start small: Book that overdue check-up this month. Many women find peace of mind after a normal result — and early detection offers the best path forward if anything needs attention.
Imagine feeling more in control of your health, knowing you’re taking steps backed by science.
FAQ
What is the most common sign of cervical cancer? Unusual vaginal bleeding, such as between periods or after intimacy, is frequently mentioned by health experts as a key change to notice.
Can cervical cancer be prevented? Yes — regular screening and HPV vaccination (when recommended) are two of the strongest ways to lower risk, according to major health organizations.
When should I see a doctor about these signs? Any persistent change, especially unusual bleeding or pain, should prompt a visit. It’s always better to get checked than to wonder.
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider if you have concerns about your health or experience any symptoms.