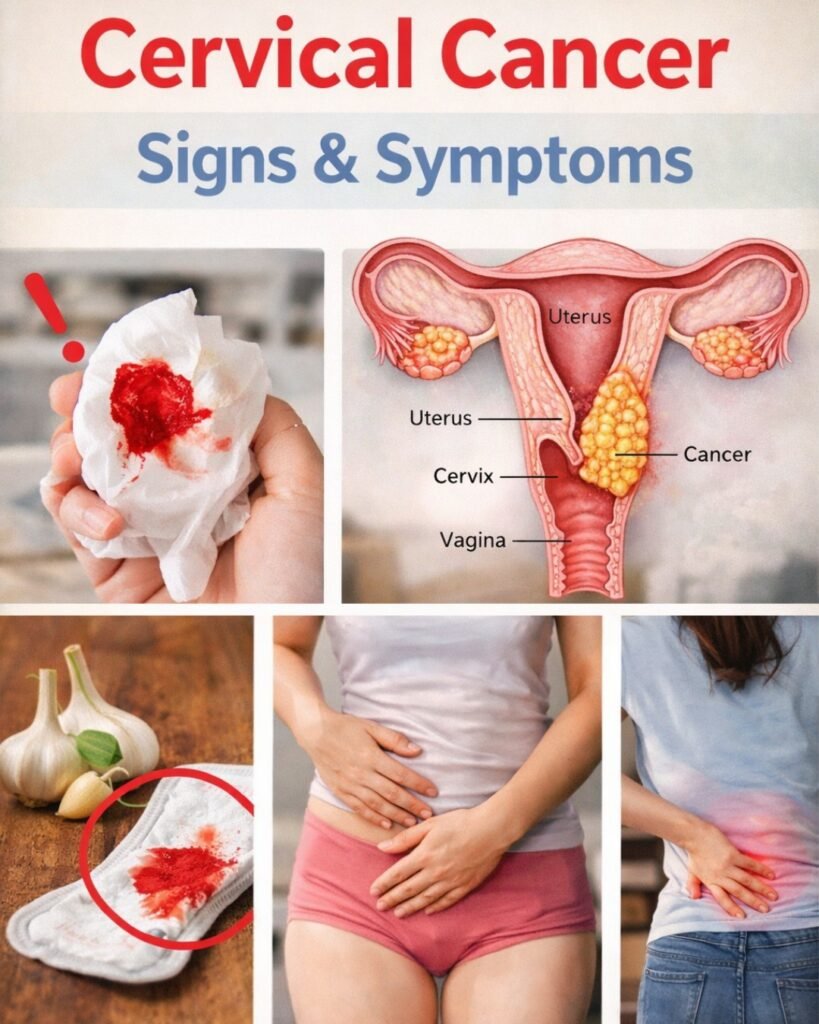
Cervical cancer is a silent predator that affects thousands of women annually, yet its earliest whispers are frequently dismissed as mere side effects of aging, stress, or a busy lifestyle. When you are juggling a career and family in your 40s or 50s, a nagging pelvic ache or a slight change in your body’s rhythm seems like something that can wait until tomorrow. Unfortunately, delaying care turns manageable concerns into life-altering challenges, leaving many women feeling isolated and wondering if they are simply overreacting to “vague” symptoms. By the time the realization hits that something is truly wrong, the window for the most effective early intervention may have already narrowed.
But what if you could regain control by simply knowing exactly what to look for? There is a profound sense of empowerment that comes from turning on the light in a dim room and seeing the path clearly. In the next few minutes, we will reveal the nine specific signals your body uses to alert you to cervical changes—including one “hidden” symptom that most women never associate with reproductive health.
The Silent Evolution: Why We Miss the Signs
Cervical cancer often develops slowly over several years. During this pre-cancerous stage, the body sends out subtle flares. The problem is that these flares mimic common issues like hormonal fluctuations or minor infections.
According to major health organizations, over 14,000 women in the U.S. are diagnosed each year. However, when caught early, the survival rate increases dramatically. To stay protected, we must look past the “normal” and identify the persistent patterns.
9. Unusual Vaginal Discharge with a Different Texture
Many women, like Sarah, a 48-year-old teacher, notice a watery or sticky discharge and assume it’s just perimenopause. While discharge changes throughout your cycle, a specific type of shift warrants a second look.
Scientific research suggests that when cervical cells begin to change abnormally, they may produce a watery, bloody-tinged, or foul-smelling discharge. This isn’t just about “wetness”; it’s about a persistent change in odor and consistency that doesn’t go away with standard hygiene.
But here is the catch: If the discharge has a pale, watery appearance or a faint metallic scent, it could be a sign of cellular shedding. Don’t just brush it off as a “pH imbalance.”
8. Pain or Discomfort During Intimacy
Discomfort during sex is often attributed to vaginal dryness or aging. However, Lisa, 52, described a sensation like “sandpaper” that felt deeper than just surface irritation.
Medical journals indicate that cervical abnormalities can make the tissue more fragile. When this tissue is touched, it can lead to pain or even light bleeding. This is often linked to inflammation or the development of small growths on the cervix.
- The Red Flag: Pain that occurs consistently during or after intimacy.
- The Reality: While lubrication issues are common, persistent deep pain is a signal to see a professional.
7. Abnormal Bleeding Between Periods
This is perhaps one of the most significant “red alerts.” Emily, 46, noticed spotting on her underwear even though her period wasn’t due for two weeks. She blamed stress, but the spotting continued.
Data from the CDC confirms that bleeding outside your normal cycle—or any bleeding after you have reached menopause—is not normal. Research involving thousands of women links this irregular spotting to HPV-related changes in the cervical lining.
Think about it this way: Your body follows a rhythm. When that rhythm breaks without a clear cause, it’s an invitation to investigate.
6. Persistent Pelvic Pain That Lingers
We all experience occasional cramps, but Maria, 50, felt a dull throb in her lower abdomen that felt like a “heavy weight.” It wasn’t the sharp pain of a period; it was a constant pressure that made sleep difficult.
Clinical reviews connect ongoing pelvic discomfort to the pressure cervical changes can place on nearby tissues. As cells grow, they may take up space or cause inflammation in the pelvic cavity.
Expert Note: If you find yourself reaching for painkillers every day for “unexplained” pelvic heaviness, it’s time to stop treating the symptom and find the cause.
5. Unexplained Fatigue That Drains Your Energy
We live in a tired society, but “oncology fatigue” is different. Anna, 47, felt a bone-deep tiredness that a cup of coffee couldn’t fix. She felt exhausted by midday despite sleeping eight hours.
Studies from the National Cancer Institute suggest that the immune system uses a massive amount of energy to fight off abnormal cell growth. This can result in a systemic feeling of depletion.
But wait, there’s more… Fatigue is often the most ignored symptom because we wear busyness as a badge of honor. If your “tired” feels “heavy,” listen to it.
4. Sudden Weight Loss Without Trying
While many of us welcome a few lost pounds, unexplained weight loss is a metabolic warning sign. Rebecca, 49, saw the numbers on the scale drop even though her diet hadn’t changed.
Health experts note that when the body is under stress from cellular abnormalities, it may prioritize energy for the immune response, leading to a suppressed appetite or changes in how nutrients are absorbed.
- Significant Loss: A drop of 5% or more of your body weight in 6-12 months without trying.
- Action Step: Monitor your weight weekly if you feel other symptoms on this list.
3. Lower Back Pain That Won’t Quit
This is where it gets sneaky. Sophia, 51, thought her backache was from gardening. But the pain wasn’t in her muscles; it was a deep, radiating ache in the small of her back.
Medical literature ties chronic lower back pain to cervical issues when the growth begins to press against the nerves of the spine or pelvic wall.
Here is the interesting part: Most people head to a chiropractor for back pain. If the adjustments don’t work, the source might be internal rather than skeletal.
2. Swelling in the Legs or Feet (Edema)
Imagine your ankles puffing up by the end of the day, leaving the skin tight and shiny. Laura, 53, thought she was just standing too much at work.
The truth? If a cervical growth becomes large enough, it can press against the lymphatic vessels or veins in the pelvic region. This obstructs fluid flow, causing it to pool in the legs and feet.
Key Difference: Normal swelling usually goes down overnight with elevation. If your swelling persists even after rest, it requires medical attention.
1. Urinary Problems and Frequent Urges
The most common sign that women overlook is a change in bladder habits. Karen, a 45-year-old nurse, felt a constant urge to urinate and a burning sensation. She thought it was just a UTI or too much caffeine.
Scientific insights reveal that because the bladder and cervix are neighbors, any change in the cervix can put immediate pressure on the bladder. This results in frequency, urgency, or even a “leaking” sensation.
Comparing Common Issues vs. Cervical Warning Signs
To help you differentiate, refer to this comparison table:
| Sign | Common/Benign Cause | Potential Cervical Link |
| Unusual Discharge | Hormonal shifts, yeast infection | Cellular changes causing “fishy” odor or watery tint |
| Pain During Sex | Lack of lubrication, aging | Tissue inflammation or cervical growths |
| Spotting | Stress, missed birth control | HPV-related abnormalities in the lining |
| Pelvic Pain | Muscle strain, ovulation | Tissue pressure from abnormal cell growth |
| Back Pain | Poor posture, heavy lifting | Nerve involvement or pelvic congestion |
| Leg Swelling | Salty diet, long flights | Lymphatic blockage from pelvic pressure |
Export to Sheets
Your Action Plan: What to Do Next
If you recognize one or more of these signs, don’t panic. Panic paralyzes, but action empowers. Follow these steps to safeguard your health:
- Start a Symptom Journal: Track the duration, frequency, and triggers of your symptoms for 2 weeks.
- Schedule a “Well-Woman” Exam: Contact your gynecologist and specifically ask for a Pap test and an HPV test.
- Review Your History: Check when your last screening was. If it has been more than 3 to 5 years, you are due.
- Lifestyle Support: Focus on a high-antioxidant diet (think berries, leafy greens, and garlic) to support your immune system while you wait for your appointment.
Conclusion: Turning Awareness into Protection
Recognizing these nine signs is like catching a whisper before it becomes a shout. Women like Sarah and Karen found their way back to health not because they were lucky, but because they chose to listen to their bodies instead of silencing them.
The three most critical takeaways are: pay attention to persistent discharge, never ignore post-menopausal or mid-cycle bleeding, and treat chronic pelvic pressure as a valid medical concern.
What is the one small step you can take today? Perhaps it’s calling your doctor or sharing this article with a friend. That one conversation could be the light that changes everything.
Frequently Asked Questions (FAQ)
1. Can I have cervical cancer even if my Pap smear was normal last year? While Pap smears are highly effective, they are not 100% foolproof. If you have persistent symptoms like abnormal bleeding or pain, you should request a follow-up or an HPV test, even if your last screening was clear.
2. Is HPV the only cause of cervical cancer? High-risk strains of HPV are responsible for the vast majority of cases. This is why the HPV vaccine and regular testing are the most powerful tools for prevention.
3. At what age should I stop worrying about cervical cancer? Screening guidelines usually suggest continuing until age 65, but symptoms should never be ignored at any age. Post-menopausal bleeding is always something that needs to be checked by a doctor.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.