About 13,500 new cases of cervical cancer are diagnosed in the United States each year, and around 4,200 women lose their lives to this disease—yet it’s one of the most preventable cancers when caught early. Many busy women in their 30s, 40s, and beyond dismiss subtle body changes as “just stress,” hormonal shifts, or normal aging, allowing potential issues to progress quietly. The frustrating part? These overlooked clues can delay vital care, making treatment harder and outcomes less certain. But here’s the empowering truth: recognizing these signs early can lead to timely intervention and peace of mind. Keep reading—you’ll discover the 9 critical warning signs most women miss, real stories of early action, and practical steps that could change everything.
The Silent Threat: Why Cervical Cancer Often Goes Unnoticed
Cervical cancer develops slowly, often without dramatic symptoms in its early stages. Persistent infection with high-risk types of human papillomavirus (HPV)—a common virus spread through sexual contact—drives nearly all cases.
Research from the American Cancer Society shows that regular screening has cut cervical cancer rates by more than 50% over recent decades. Yet thousands of cases still occur annually, often because vague symptoms get ignored.
Sound familiar? That unexpected spotting or lingering discomfort you chalked up to a busy life?
You’re not alone. Many women prioritize everything else before their own health. But listening to your body now can make a real difference.
Ready to sharpen your awareness? Let’s dive in.
Why These Early Signs Matter—and the Role of HPV
HPV is extremely common—most sexually active people encounter it at some point. In most cases, the body clears it naturally. But when high-risk strains persist, they can lead to cell changes in the cervix over time.
The challenge? Early cervical changes rarely cause obvious symptoms. When signs do appear, they’re often subtle and easy to dismiss.
Studies highlight that early detection through awareness and screening dramatically improves survival rates—often to near 100% when found in precancerous stages.
But that’s not all…
These signs can disrupt daily life, intimacy, and confidence if ignored. The good news? Knowledge empowers you to act sooner.
Let’s explore the 9 signs most women overlook.
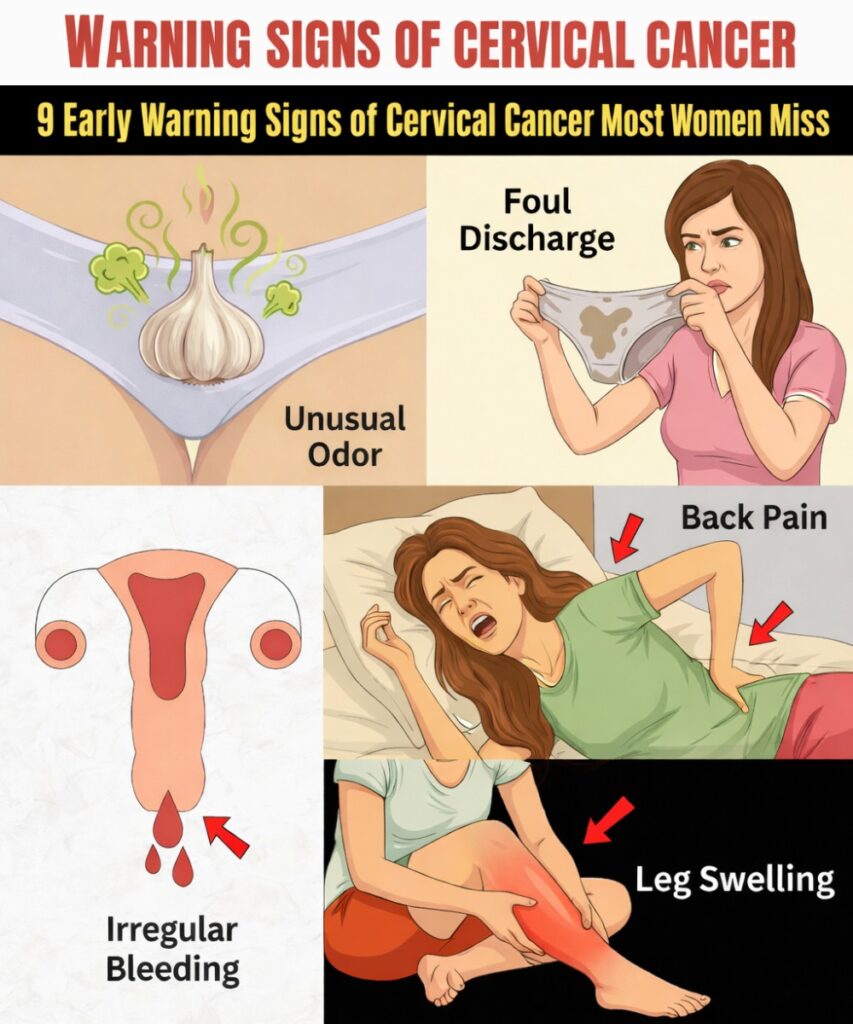
Sign 1: Abnormal Vaginal Bleeding That Doesn’t Fit Your Normal Pattern
Unexpected spotting between periods, after intercourse, or even light bleeding after menopause—these can feel alarming yet easy to brush off.
Take Emily, a 38-year-old office manager: “I noticed bleeding after sex and thought it was just irritation. I almost waited it out.”
Abnormal bleeding is one of the most common early alerts, often linked to changes in cervical tissue.
Emily finally saw her doctor. Tests caught precancerous cells early, and simple treatment resolved it. “Acting quickly gave me huge relief,” she shared.
If you’ve noticed this, rate its frequency on a scale of 1-10. Anything above 3 deserves attention.
Bonus tip: Track your cycles in an app—patterns become clearer.
Sign 2: Unusual Vaginal Discharge
A sudden increase in discharge that’s watery, bloody, pink, or has a strong odor can catch you off guard.
Sarah, a 41-year-old nurse, recalls: “Mine became heavy and foul-smelling. I assumed it was an infection and self-treated.”
Persistent unusual discharge can signal cervical changes or related issues.
Sarah got checked—early intervention restored normalcy and eased her worries.
Self-check: Have you noticed changes lately? Don’t ignore them.
But wait—there’s another intimate sign many avoid discussing…
Sign 3: Pain or Discomfort During Intercourse
When intimacy starts to hurt or feel uncomfortable, it’s tempting to avoid the topic—or the activity.
Lisa, 39, shared: “Sex became painful, and it strained my relationship. I thought it was temporary.”
This can stem from cervical changes causing inflammation or pressure.
Lisa spoke up during a checkup. Addressing it early brought back comfort and closeness.
Quick reflection: How’s your comfort level lately?
You’re already ahead of most readers—keep going.
Sign 4: Persistent Pelvic Pain or Pressure
A dull ache, heaviness, or ongoing discomfort in the lower abdomen that lingers?
Rachel, 42, said: “I blamed constant pelvic pressure on stress and long work hours.”
This can indicate growing changes pressing on nearby tissues.
Rachel’s imaging and prompt care resolved it. “I finally felt like myself again.”
Rate any pelvic discomfort 1-5. Lingering pain isn’t “normal.”
Sign 5: Longer or Heavier Menstrual Periods
Suddenly heavier flows or periods that drag on longer than usual?
Anna, 37, noticed: “My periods became exhausting—heavy bleeding wiped me out.”
Cell changes can disrupt normal hormonal signals.
Anna’s investigation caught issues early, making management straightforward.
Insider tip: Log your cycles monthly. Trends matter.
Sign 6: Any Bleeding After Menopause
Post-menopausal spotting or bleeding is never “normal.”
Karen, 52, panicked: “I thought periods were over forever—then spotting started.”
This is a classic red flag warranting immediate evaluation.
Karen’s quick action led to early intervention and better outcomes.
Sign 7: Unexplained Fatigue or Weakness
Ongoing tiredness that rest doesn’t fix?
One woman’s partner noticed constant exhaustion she attributed to a busy life.
Systemic effects from advancing changes can contribute.
Supportive care and early attention helped restore energy.
Sign 8: Leg Pain or Swelling
Unexplained pain or swelling in one or both legs.
This can signal pressure on blood vessels or lymph nodes.
Monitor closely and discuss with your provider.
Sign 9: Changes in Urinary or Bowel Habits
Frequent urges, difficulty urinating, or bowel changes without clear cause.
These may indicate pressure from nearby growth.
Professional evaluation is key.
You’ve made it through all 9 signs—great job staying engaged!
Common Early Signs at a Glance
| Sign | Common Dismissal | Why It Matters |
|---|---|---|
| Abnormal Bleeding | “Just irregular periods” | Often the first noticeable alert |
| Unusual Discharge | “Probably an infection” | Can indicate tissue changes |
| Pain During Sex | “Temporary issue” | May signal inflammation or growth |
| Pelvic Pain | “Stress or aging” | Possible pressure on nearby tissues |
Your Best Defense: Prevention and Early Detection
HPV vaccination prevents most high-risk strains—ideally before sexual debut, but beneficial up to age 45.
Quitting smoking, maintaining a healthy weight, and practicing safe sex also lower risk.
But screening remains the gold standard.
Current Screening Guidelines (2025–2026)
| Age Group | Recommended Screening | Frequency |
|---|---|---|
| 21–29 | Pap test alone | Every 3 years |
| 30–65 | Pap + HPV co-test, or HPV test alone | Every 5 years |
| 65+ | May stop if prior tests normal | Consult provider |
Always discuss your personal risk factors with your doctor.
Actionable Steps You Can Take Today
- Schedule your next screening if overdue.
- Talk openly with your provider about any symptoms.
- Get the HPV vaccine if eligible.
- Track symptoms and cycles in a journal or app.
- Share this information with women you care about.
Imagine the peace of mind 30 days from now—knowing you’re proactive and protected.
Final Thoughts: Empowerment Through Awareness
Cervical cancer is largely preventable with vaccination, regular screening, and attention to your body. Early action leads to the best outcomes and preserves your quality of life.
You’ve gained valuable knowledge today—use it.
Thousands of women prioritize these steps every year. Join them.
Quick FAQ
At what age should I start cervical cancer screening?
Most guidelines recommend starting at age 21 or 25, depending on the specific recommendations—talk to your doctor.
Can cervical cancer be prevented completely?
While not 100% preventable, HPV vaccination and regular screening prevent the vast majority of cases.
What should I do if I notice one of these signs?
Contact your healthcare provider promptly for evaluation—early discussion is always better.
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider for personalized guidance regarding symptoms, screening, or health concerns.